If you’re like most people, you’ve probably never heard of the parathyroid glands. Most people think of the thyroid, but don’t get caught up in the idea that the parathyroid glands and thyroid glands have anything to do with one another.
They’re located right on top of each other and have similar names, but they serve completely different roles and have no other relation beyond that of friendly neighbours.
While your parathyroid glands may take a deep backseat to any discussion you’ve ever had about health, they are not to be taken lightly – because they will not take a backseat in regards to your physiological functioning.
These four tiny yellow glands, which are about the size of rice grains, are found behind the thyroid on your neck, and their main purpose is to produce parathyroid hormone (PTH), signalling molecules that regulate your internal balance of calcium and phosphorous.
This is Important Work, to be Sure.
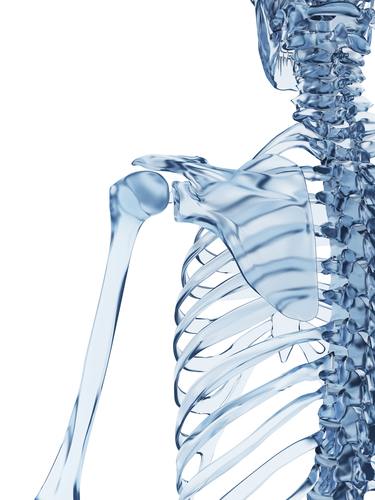
They’ve preached at you about calcium your entire life. It’s for bones. Strong, dense bones.
You know this stuff, but it’s so easy to take your body’s complexity for granted. So to clarify, bones not only provide support for all your tissues but protect your organs, produce red and white blood cells, allow you to stay mobile, and store essential minerals. Calcium is actually a soft metal, and it’s highly important to cell physiology as well, sparking cellular processes and mineralizing bones and teeth.
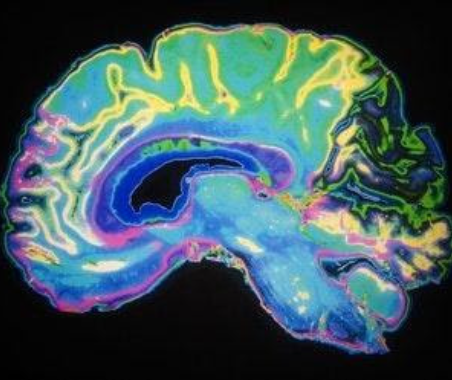
Calcium is also the primary element in muscle contraction and helps conduct the electrical currents along your nerves.
Think about how you get a tingly feeling in your fingers or when your hand cramps up – this often occurs when calcium levels are low, which creates a pretty stark picture of just how integral a role this stuff plays in your body’s functioning.
But more is not better. High calcium can really beat you down. You get lousy sleep. You get crabby. You get forgetful.
And that’s just for starters.
Let’s look closer.
The Different Types of Parathyroid Disorders
Parathyroid Disorders come in two forms, neither of them pleasant.
The “other” parathyroid disorder is hypoparathyroidism. We’ll refer to it as such because it is far rarer and not really the topic of this article. This condition occurs when the parathyroid glands aren’t producing enough PHT to maintain proper calcium levels, and the result is low calcium in the blood. The reasons are sometimes genetic but more often the result of surgery on the thyroid or parathyroid glands (perhaps to correct a hyperparathyroidism disorder).
It can also be caused by damage to the immune system.
Sufferers will often experience cramps and muscle twitches.
Hyperparathyroidism is a far more likely scenario for the average American citizen. As the name suggests, hyperparathyroidism refers to overproduction of PHT.
There are also two different kinds of hyperparathyroidism.
The first, primary hyperparathyroidism is a gland malfunctioning issue that creates high levels of calcium. Essentially, the gland isn’t functioning the way it should. One or more of them isn’t listening to the signals sent by your body to put the production brakes on.
Often, the reason for this is a tumor, usually noncancerous but not always. It can also be caused by an enlarged gland.
Secondary hyperparathyroidism doesn’t have anything to do with the glands. Rather, it’s the source of the signal that’s creating the problem, and you have to go the source to find out what’s happening.
A common cause is a low amount of calcium in your body because you’re not getting enough in your diet (or not absorbing it properly) or enough Vitamin D from food or the sun (1).
Chronic kidney disease, kidney failure, and kidney transplants can also cause this problem. Your kidneys help turn D into a useable form, so if they don’t work, you have less Vitamin D available and calcium decreases (2).
Secondary hyperparathyroidism can also be a result of gastric bypass surgery (2).
Symptoms and Dangers of Untreated Hyperthyroidism
While the existence of these conditions may be seldom discussed, the outcome is nothing to take lightly. They are often referred to as the “moans, groans, stones, and bones.” Or, to be more specific, emedecine.com offers “painful bones, renal stones, abdominal groans, and psychic moans” as a mnemonic (3).
All this may make it sound worse than it feels. Generally, sufferers don’t notice much and may even claim to feel fine when they are diagnosed with a parathyroid disorder. But after they’ve been treated, they’ll also say they feel a lot better.
EndocrineWeb.com reports (4), “Many patients who thought they were asymptomatic pre-operatively will claim to sleep better at night, be less irritable, and find that they remember things much easier than they could when their calcium levels were high.”
It’s this subtle nature of the condition that often leaves it untreated, and lack of treatment can cause horrifying problems. For one, severe calcium overproduction builds up so much that bones become brittle and a lot easier to break. When the overactive parathyroid glands start releasing excess PTH, the bones dump calcium into the bloodstream to get rid of it. Osteoporosis ensues – there’s your painful bones.
The disorder is also associated with kidney stones, due to the calcium-rich blood filtered through the kidneys.
Gastric ulcers and pancreatitis are the abdominal groans in the emedicine mnemonic. The excess calcium is destructive to cells and thus affects the pancreas and stomach lining, leading to pain and inflammation. In the worst case scenario, kidneys can start becoming hard like and even fail.
Nervous system problems explain the psychic moans. Patients will get tired easily and feel fatigued and weak. They’ll forget a lot of stuff. They’ll feel ill or depressed for no observable reason.
Additional symptoms to watch out for include nausea, vomiting, low appetite, and excessive urination. The risk of cardiovascular diseases might be increased by high calcium as well, and when left untreated in pregnant women, the disorder can cause low calcium problems in babies to a dangerous degree.
Are You at Risk for Hyperparathyroidism?
Parathyroid disorders are much more common in the elderly; peak incidence is between 55 and 70 (5). With the population getting older and people living longer, this could mean a drastically increasing rate of the disease. Osteoporosis and brittle bones are a major problem for the aging because they lead to a major decrease in a quality of life, reducing vitality and often leading to a premature death.
Variables that create higher risks for parathyroid disorders include menopause (for women, of course), long-term deficiencies of calcium or Vitamin D, radiation treatment, and lithium usage (for bipolar disorder) (6).
Fortunately, surgeries to correct primary hyperparathyroidism are quite successful, and while older people are far less likely to get the operation, this is a mistake. A U.S. National Library of Medicine report on parathyroid surgery in the elderly states (7), “They have equivalent surgical outcomes, including morbidity, mortality, and cure rates, compared with younger patients, although their length of hospital stay is significantly longer.”
Osteoporosis Drugs and Hyperparathyroidism
Coming back to the decision many elderly people make to not get surgery, it should be made as clear as possible that osteoporosis drugs are not an effective way to treat this type of condition. They can help rebuild bone density and restore calcium after the glands are functioning normally and the excess PHT is taken out of the system, but they will do nothing until corrective action is taken (8).
Once the glands can do their job again, bone density can be regained. From Parathryroid.com (9): “Researchers at the University of Northern Sweden studied the bone density of postmenopausal women (average age 63) with primary hyperparathyroidism before and one year after parathyroidectomy [Thorsen, et al, Surgery 1997;122:882-7]. They found a significant increase in bone density in the hip and lower back one year later.”
Also, don’t forget that surgery may not be needed if you have secondary hyperparathyroidism instead of primary. In that case, and as long as the kidneys are working properly, taking in more calcium through diet and Vitamin D through diet and sunlight may be all you need to restore balance.
But, in some cases…maybe not.
Could certain circumstances render calcium and Vitamin D supplements worthless in the fight against osteoporosis?
A just released report by several of America’s top scientists and doctors says the answer is a resounding, “Yes”.
Inside the report, these health experts say that Calcium and Vitamin “do nothing” when it comes to fighting osteoporosis…
And may even trigger ‘bone death’ and cause osteoporosis!
And that instead, if you want to reverse your osteoporosis or bone disease…
All you really need to do is follow the 3 simple steps outlined on the next page…
Resources:
- http://en.wikipedia.org/wiki/Hyperparathyroidism
- http://www.mayoclinic.org/diseases-conditions/hyperparathyroidism/basics/causes/con-20022086
- http://emedicine.medscape.com/article/766906-clinical
- http://www.endocrineweb.com/conditions/hyperparathyroidism/hyperparathyroidism
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3227933/.
- http://www.mayoclinic.org/diseases-conditions/hyperparathyroidism/basics/risk-factors/con-20022086
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3227933/
- http://www.endocrineweb.com/conditions/hyperparathyroidism/hyperparathyroidism-diagnosis-treatment
- http://parathyroid.com/osteoporosis.htm
 Validating...
Validating...